In cases where a chronic anal fissure proves unresponsive to alternative treatments or if the symptoms are severe, your healthcare provider might propose surgery. The common surgical approach is known as lateral internal sphincterotomy (LIS), which entails the surgical removal of a small portion of the anal sphincter muscle. This procedure is designed to facilitate healing, diminish spasms, and alleviate pain.
Research indicates that surgery is significantly more effective than any medical intervention for chronic fissures. Nevertheless, it’s important to note that surgery carries a minimal risk of causing incontinence.
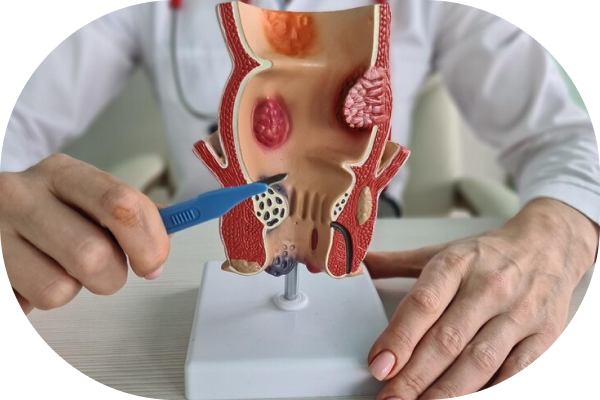
Anal fissures refer to the presence of tears or cracks in the anus, which can be mistakenly associated with hemorrhoids—swollen blood vessels located inside or just outside the anal area. Both conditions, fissures, and hemorrhoids frequently arise from the strain of passing hard stools.
Symptoms of an anal fissure?
The primary symptoms include:
- Intense pain during bowel movements.
- Sensation of burning or itching during bowel movements.
- Presence of fresh, red blood in the stool.
Additionally, certain individuals may experience:
- Spasms of the anal muscles.
- A noticeable lump on the skin near the anal tear.
Cause of an anal fissure
Injuries such as stretching and straining can lead to tears in your anal lining, while underlying conditions may also contribute. This relates to the anatomy of your anus, the terminal portion of the lengthy and muscular tube known as the large intestine.
The outer skin near the opening of your anus resembles the skin on the exterior of your body, but in the upper section where fissures commonly occur, the anus is lined with the same soft mucosa as the rest of the large intestine. This mucous lining is more delicate than regular skin, making it susceptible to tearing, particularly in infants who are prone to anal fissures. Additionally, it can become inflamed due to injury or disease, with prolonged inflammation weakening the tissues.
Surrounding your anus are two circular muscles, the anal sphincters, which assist in controlling bowel movements. If these muscles are overly tense, they can exert additional pressure on the anal lining, making it more prone to tearing and potentially reducing blood flow to the tissues.
The main factors leading to anal fissures are:
- Persistent constipation and exerting excessive pressure during bowel movements.
- Obstructed defecation syndrome.
- Infant dyschezia.
- Persistent diarrhea.
- Childbirth.
- Penetrative trauma.
Additional conditions that can contribute to anal fissures are:
- Previous surgical procedures.
- Sexually transmitted infections (STIs).
- Inflammatory bowel disease (IBD).
- Anal cancer.
- Tuberculosis (TB).
- Diaper rash.
Complications of anal fissures
While many anal fissures typically resolve on their own within a few weeks, complications can arise if they persist, referred to as chronic anal fissures. Instead of undergoing healing, these fissures perpetuate in a detrimental cycle, resulting in a persistent wound.
Pain and muscle contractions can prompt the tightening and spasming of anal muscles. This muscle tension and spasms contribute to the separation of the fissure and diminish blood flow to the tissues, impeding the healing process and intensifying pain.
When anal fissures persist without healing for an extended period, they may lead to additional complications, including:
- Fecal impaction.
- Anal stenosis (the narrowing of the anal canal, making bowel movements more challenging).
- Anal fistula.
Fissures diagnosed
A medical professional will inquire about your symptoms and attempt to visually inspect the fissure. You will be positioned lying on your stomach or side, and they will gently part your buttocks. If this causes excessive pain, further examination may be unnecessary, and they can reasonably conclude the presence of an anal fissure.
However, if you can endure the examination, they will strive to observe the fissure to eliminate other potential causes for your symptoms. This may involve the gentle insertion of a lubricated, gloved finger to open your anus, allowing them to detect any tenderness or muscle spasms. This procedure is known as a digital rectal exam.

Treatment
With proper home care, anal fissures typically recover within a few weeks. Ensure your stool remains soft by incorporating more fiber and fluids into your diet. Engage in warm water soaks for 10 to 20 minutes multiple times daily, particularly after bowel movements, to relax the sphincter and facilitate healing. If symptoms endure, additional treatment may be necessary.
Nonsurgical treatments
Your healthcare provider might suggest:
- External application of nitroglycerin (Reactive): This can enhance blood flow to the fissure, fostering healing and relaxing the anal sphincter. Nitroglycerin is typically the preferred treatment when conservative approaches prove ineffective. Possible side effects include potentially severe headaches.
- Utilizing topical anesthetic creams like lidocaine (Xylocaine) to alleviate pain.
- Injection of OnabotulinumtoxinA (Botox) to paralyze the anal sphincter muscle and ease spasms.
- Blood pressure medications such as nifedipine or diltiazem to relax the anal sphincter. These medications are usually applied topically but can also be taken orally. However, oral intake may entail greater side effects. These drugs may be considered if nitroglycerin proves ineffective or causes significant side effects.